- Solutions
used for loading font family (do’nt delete
Industries We Serve
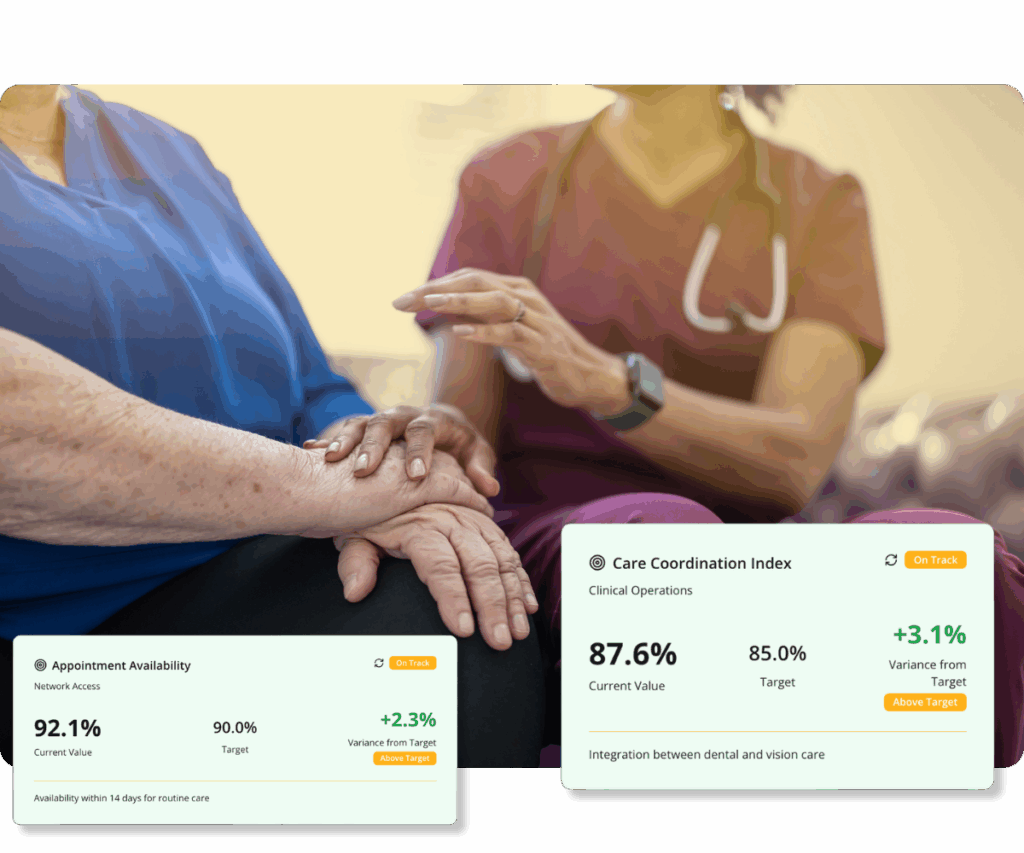
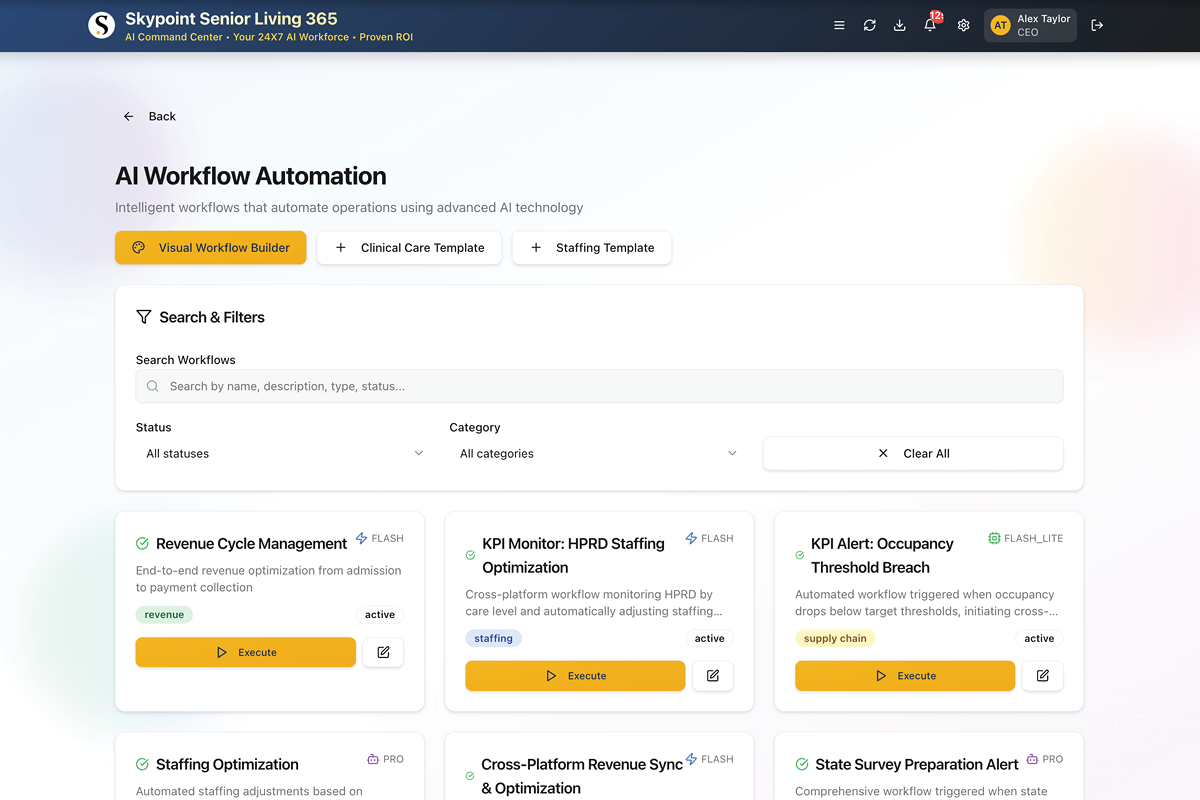
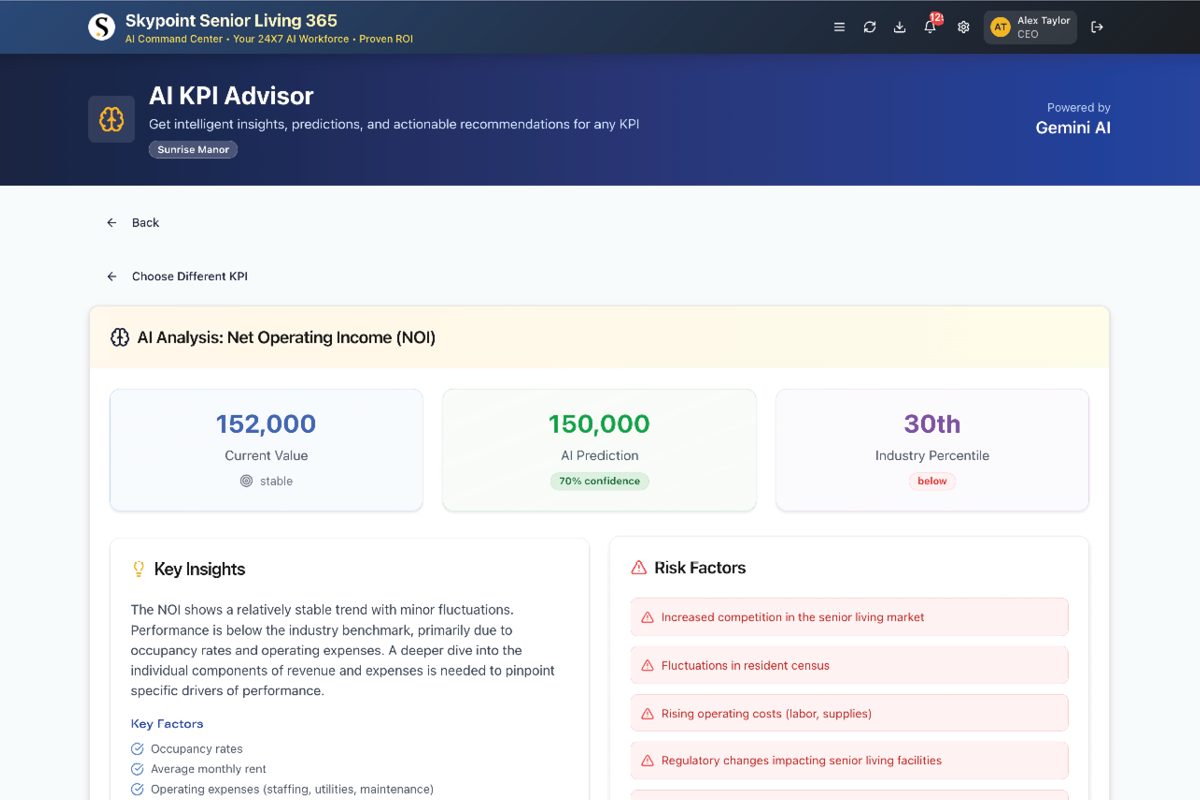
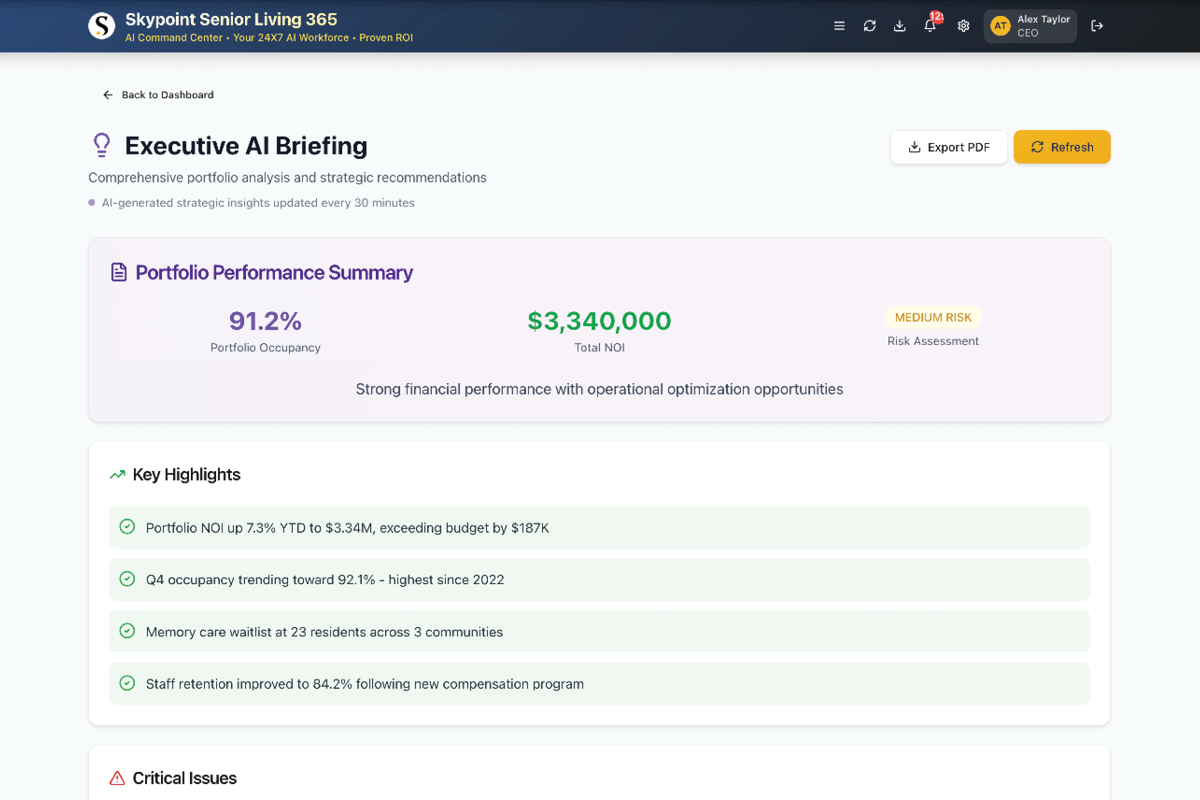
Transform siloed data into actionable intelligence. Skypoint’s AI Platform accelerates data-centric AI initiatives for healthcare, so you see results in weeks, not months.
Industries We Serve
Transform siloed data into actionable intelligence. Skypoint’s AI Platform accelerates data-centric AI initiatives for healthcare, so you see results in weeks, not months.
- Product
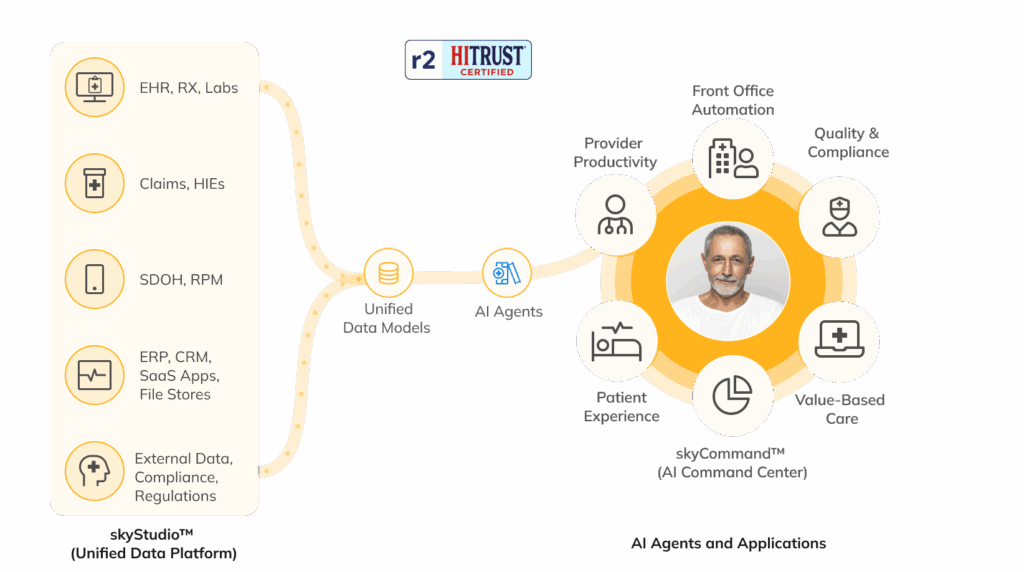
The Skypoint AI Platform
Our HITRUST r2 Certified AI Platform for the healthcare industry helps you unify your data, uncover insights, and optimize productivity.
The Skypoint AI Platform
Our HITRUST r2 Certified AI Platform for the healthcare industry helps you unify your data, uncover insights, and optimize productivity.
- Resources
Data and AI Resources
Connect with Skypoint at healthcare events, read our customer stories, and catch up on the latest AI developments on our blog.
Training and Events
Resources
Data and AI Resources
Connect with Skypoint at healthcare events, read our customer stories, and catch up on the latest AI developments on our blog.
Training and Events
Resources
- About
Who We Are
Our team of AI and BI experts helps healthcare organizations solve operational inefficiencies and enhance productivity through unified data and industry-specific compound AI systems.
About Skypoint
Contact
Who We Are
Our team of AI and BI experts helps healthcare organizations solve operational inefficiencies and enhance productivity through unified data and industry-specific compound AI systems.
About Skypoint
Contact