- Industries
Industries We Serve
Transform siloed data into actionable intelligence. Skypoint’s AI Platform accelerates data-centric AI initiatives for healthcare, so you see results in weeks, not months.
- Apps
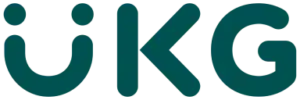
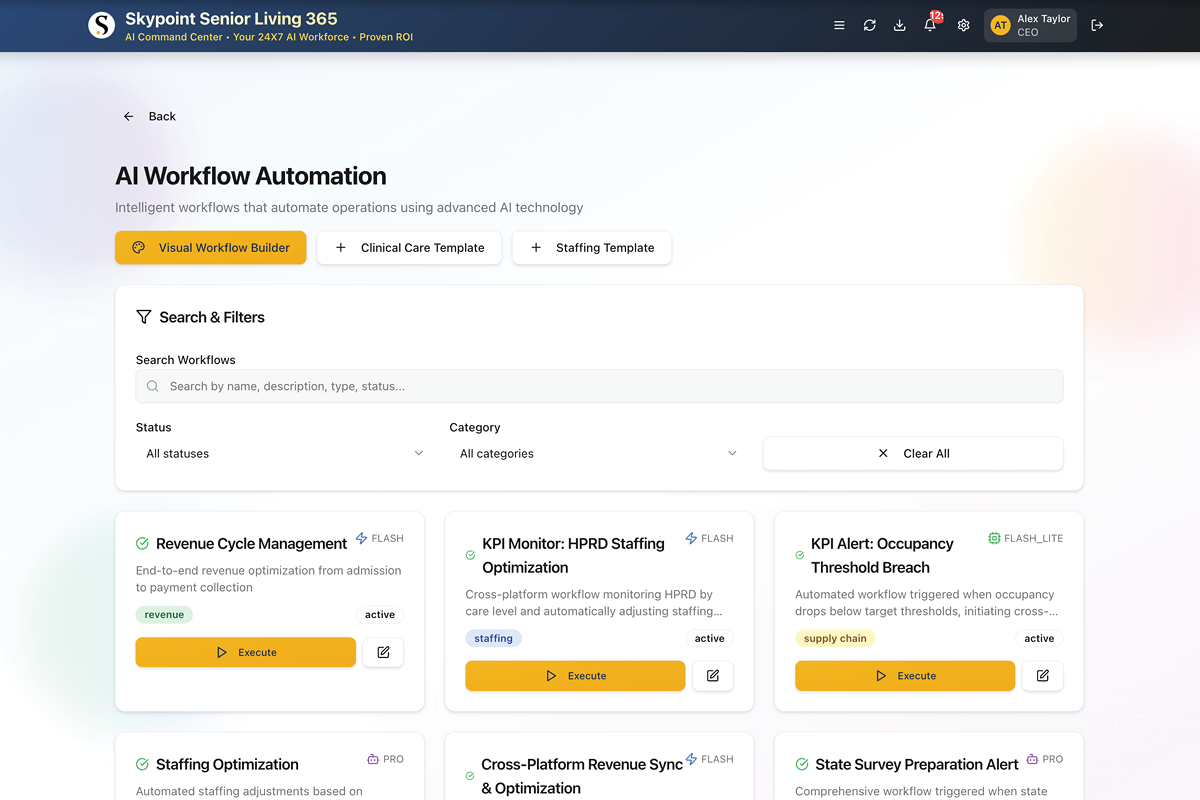
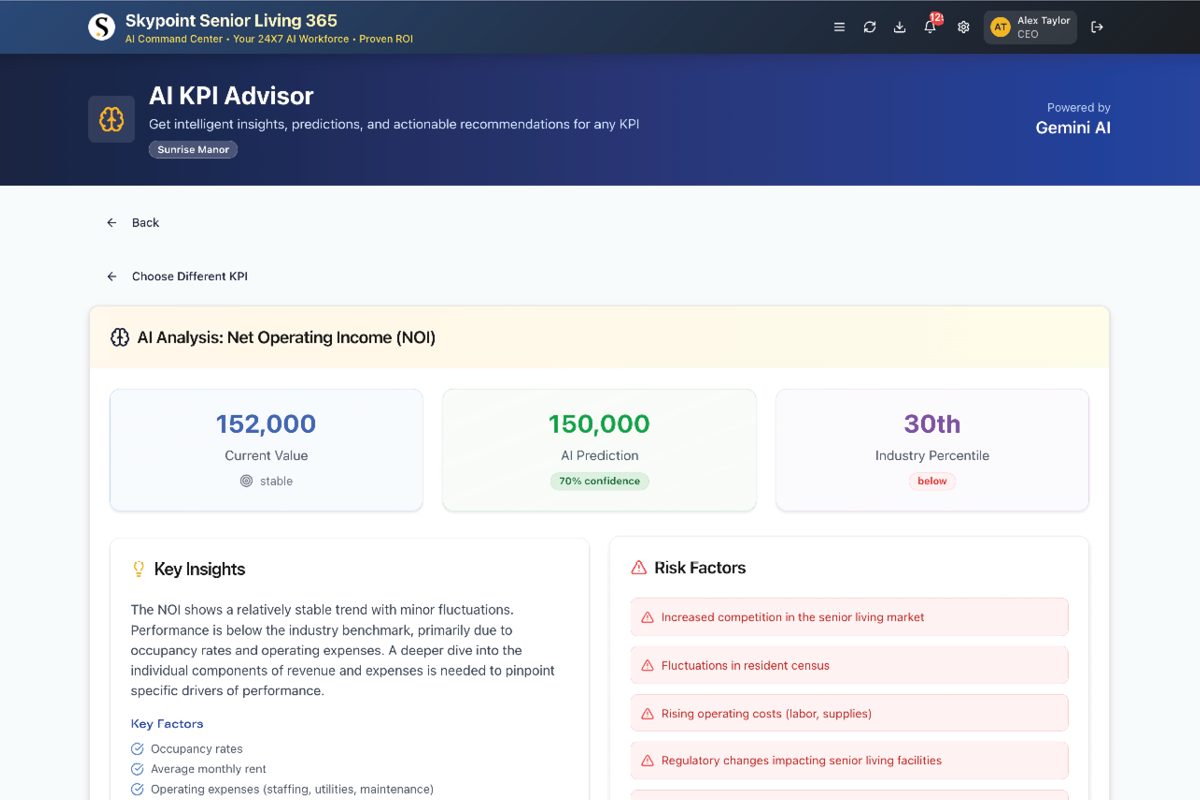
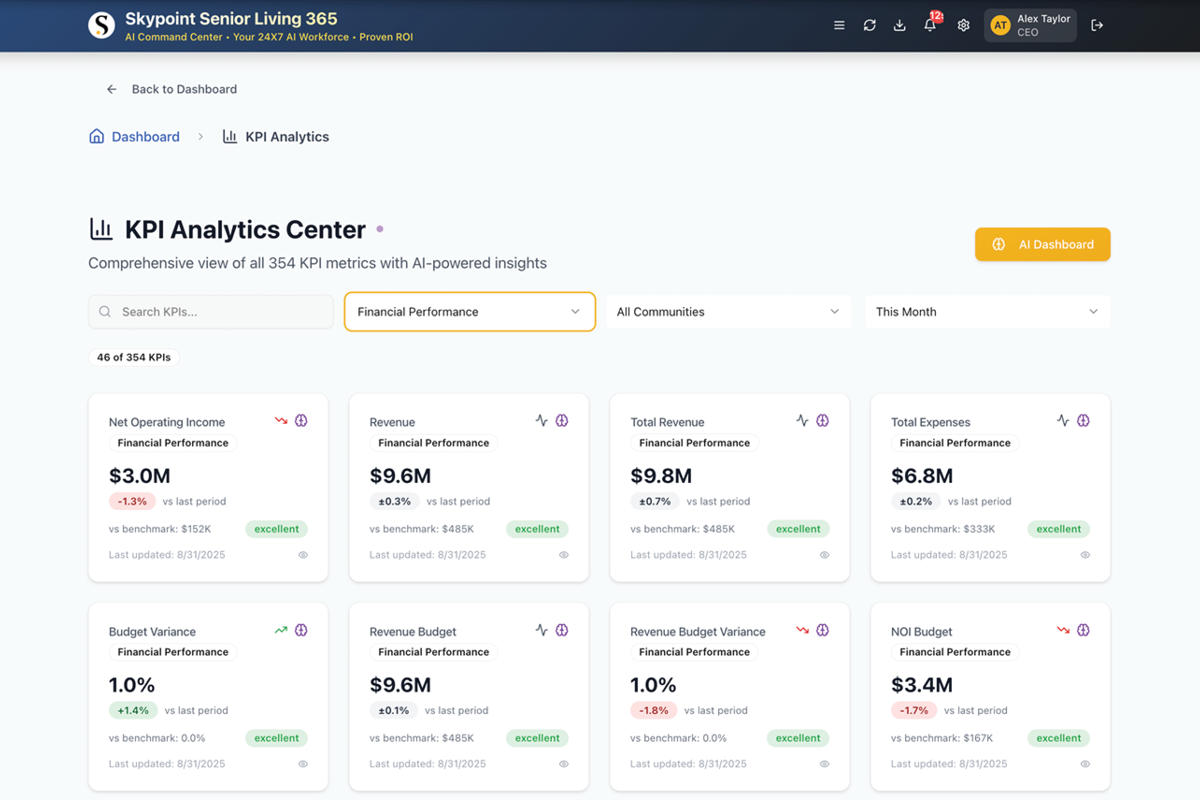
Apps
Quickly access quality data, business intelligence, analytics, and automation through Skypoint’s healthcare industry-tailored platform infrastructure.
- AI Platform
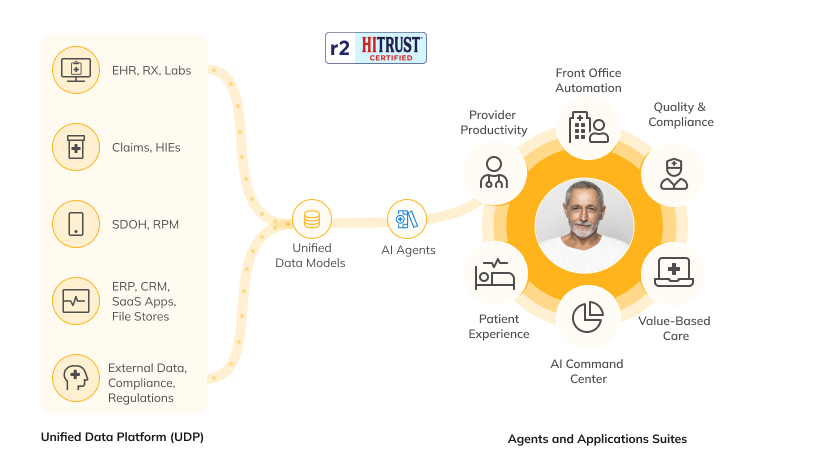
The Skypoint AI Platform
Our HITRUST r2 Certified AI Platform for the healthcare industry helps you unify your data, uncover insights, and optimize productivity.
- Resources
Data and AI Resources
Connect with Skypoint at healthcare events, read our customer stories, and catch up on the latest AI developments on our blog.
Training and Events
Resources
- About
Who We Are
Our team of AI and BI experts helps healthcare organizations solve operational inefficiencies and enhance productivity through unified data and industry-specific compound AI systems.
About Skypoint
Contact