- Solutions
Industries We Serve
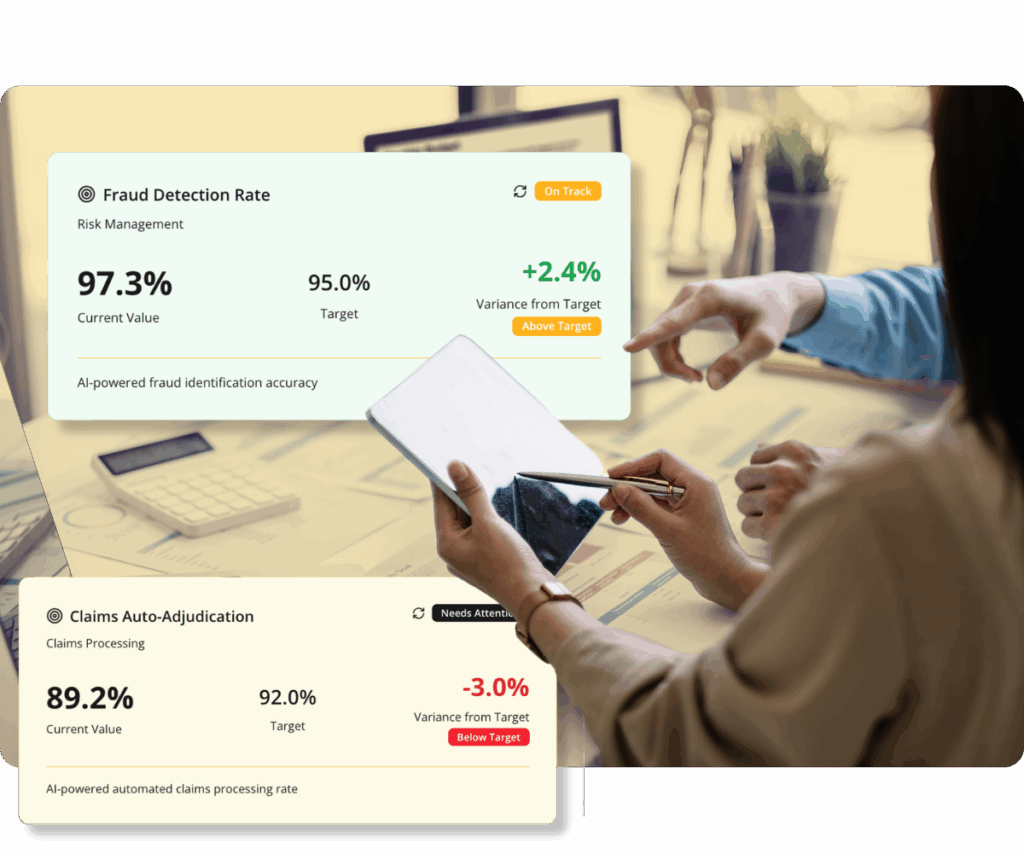
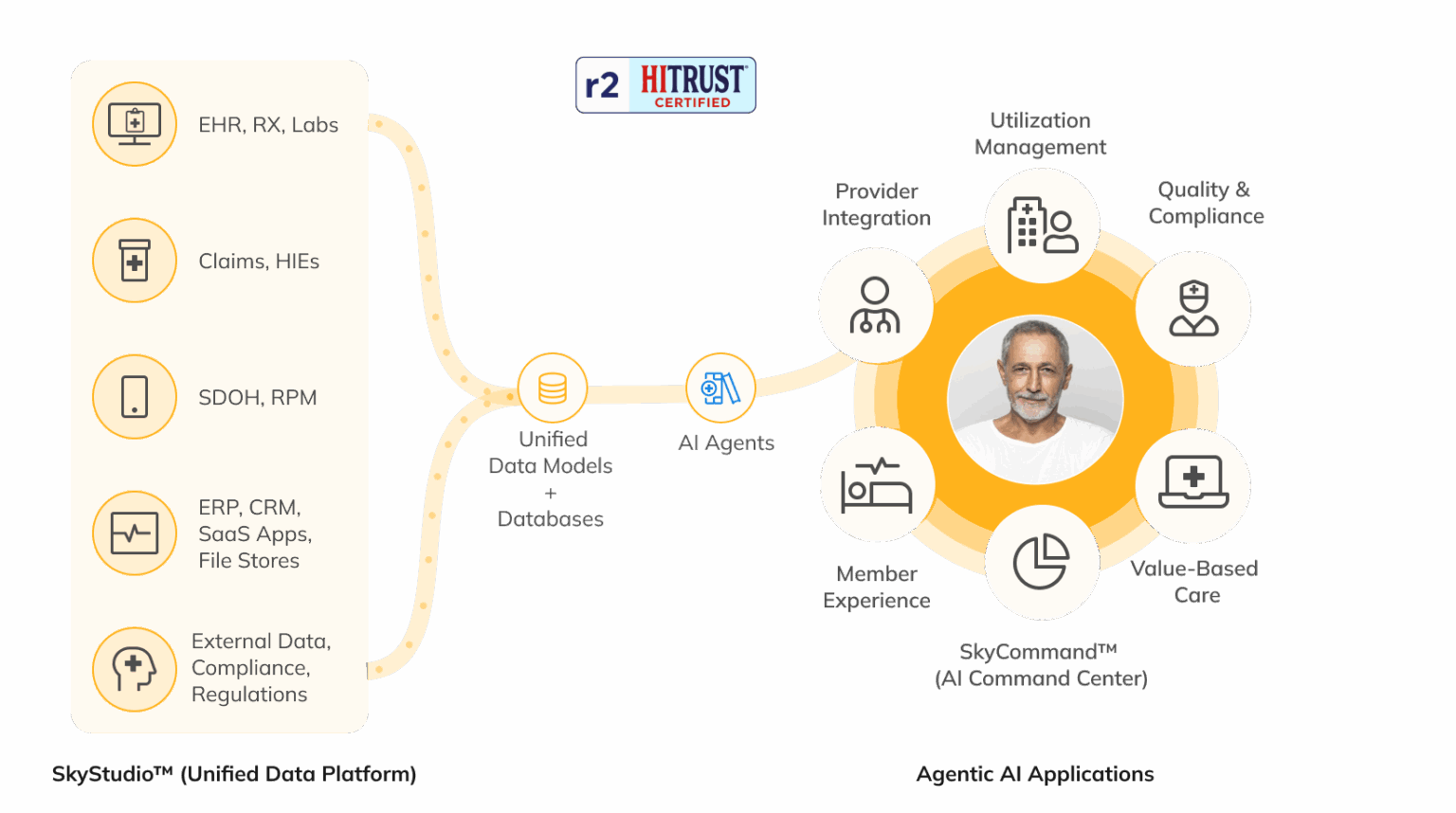
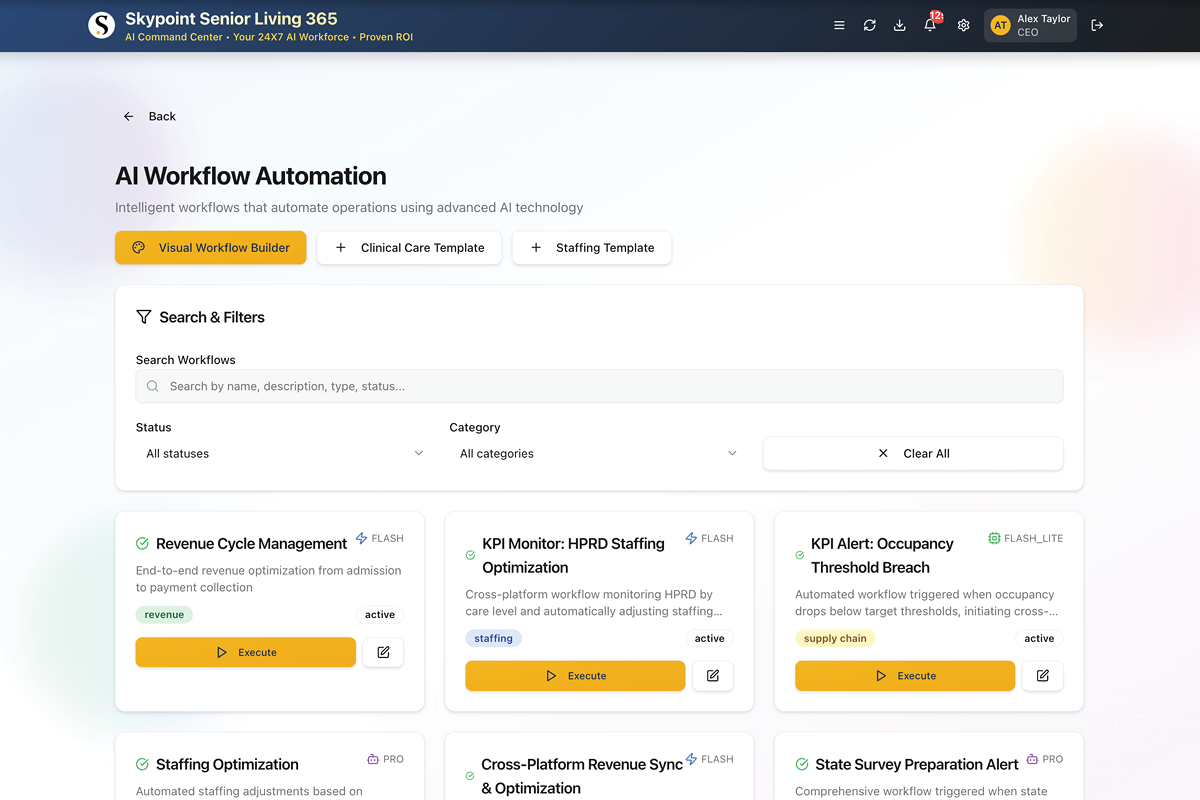
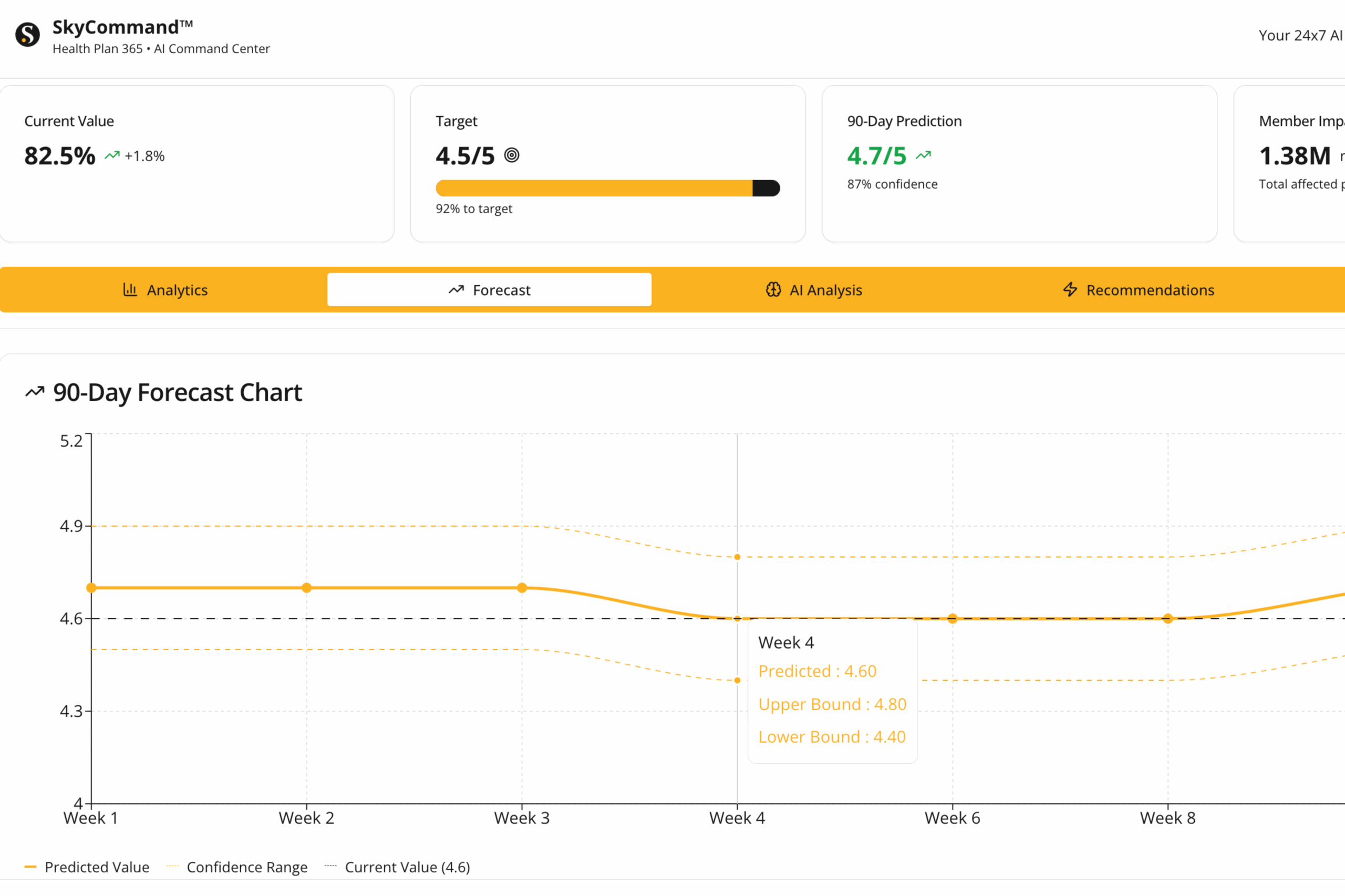
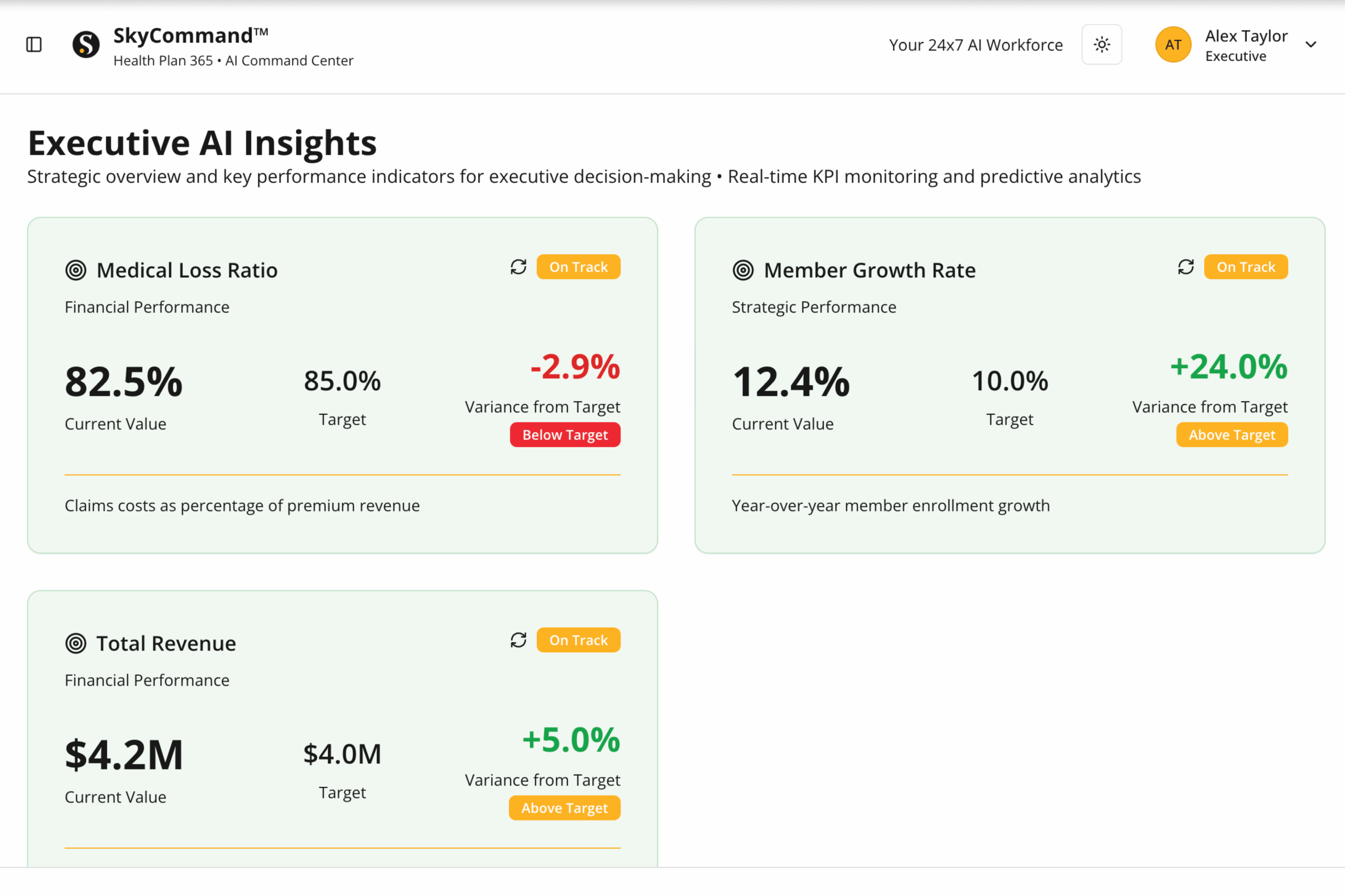
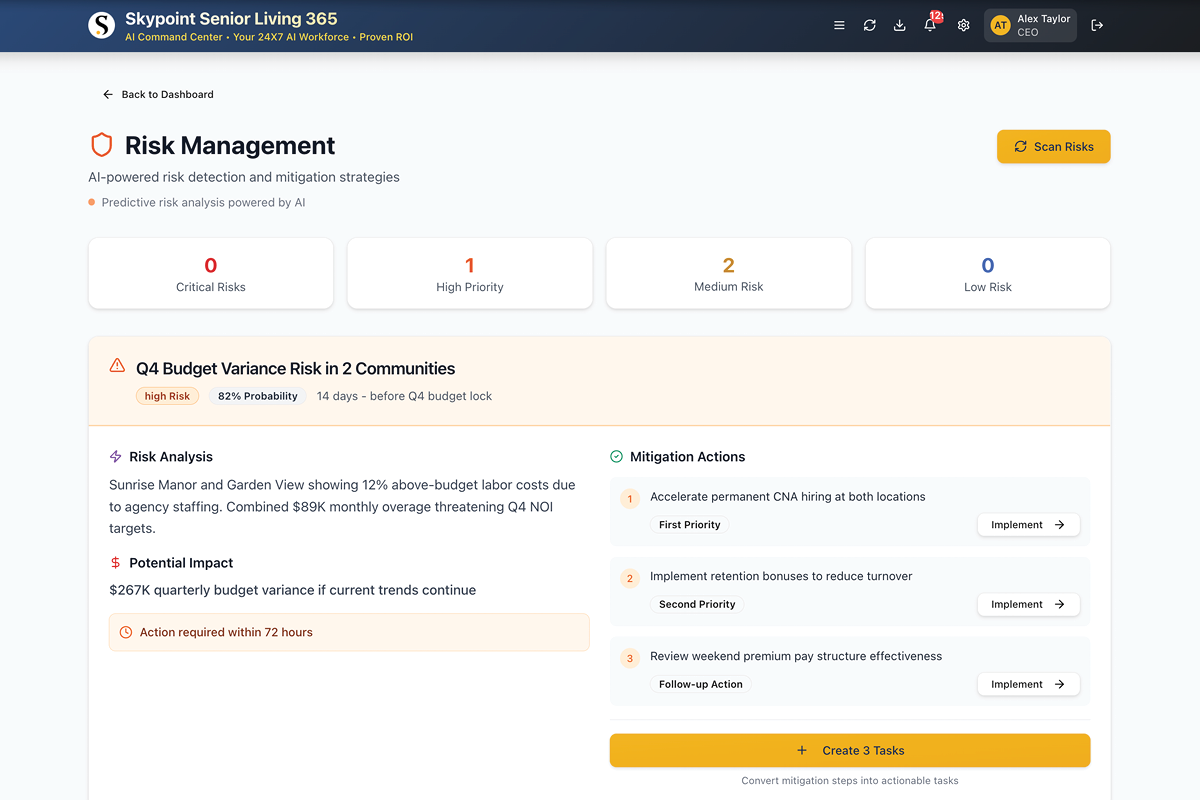
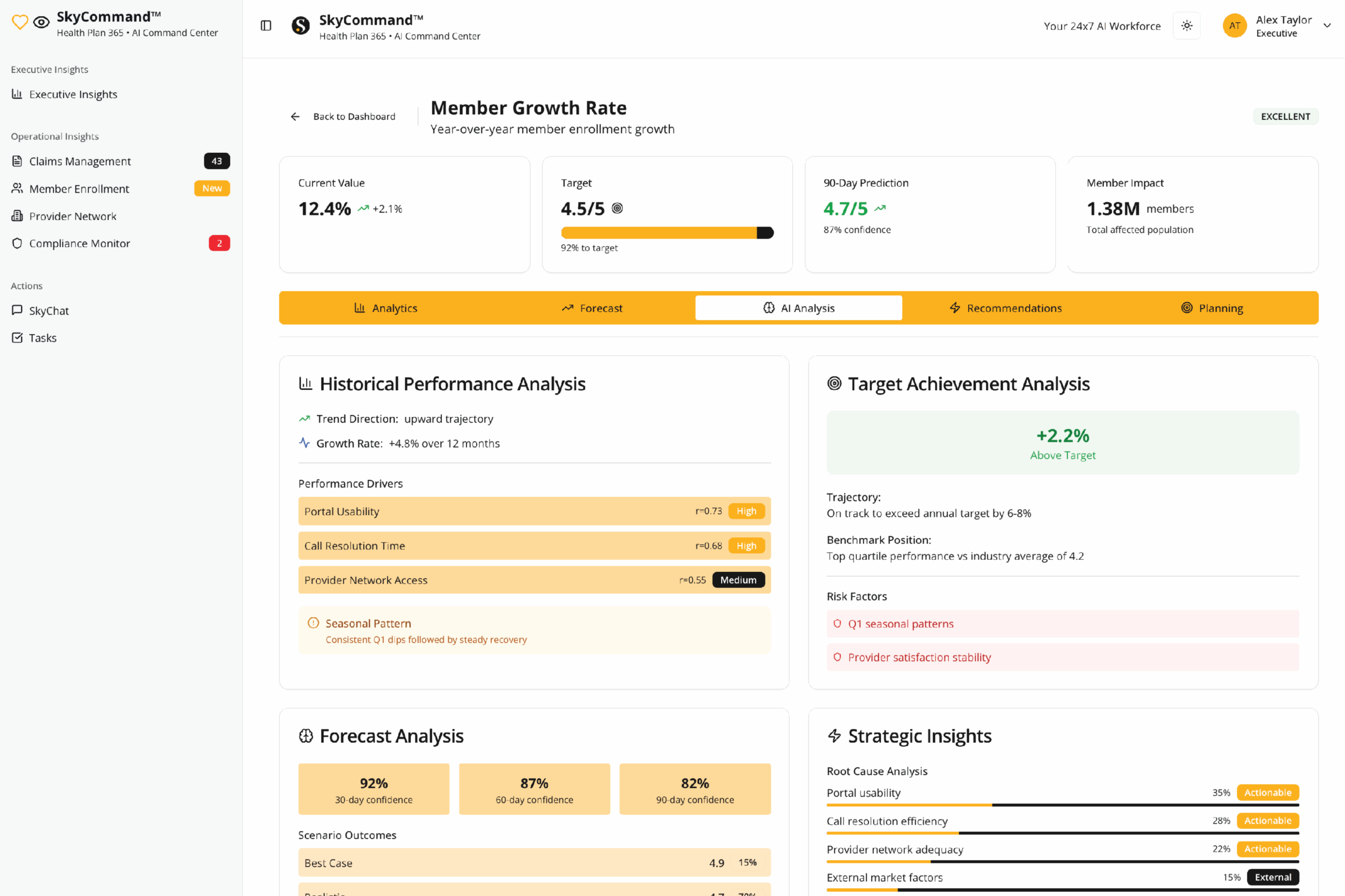
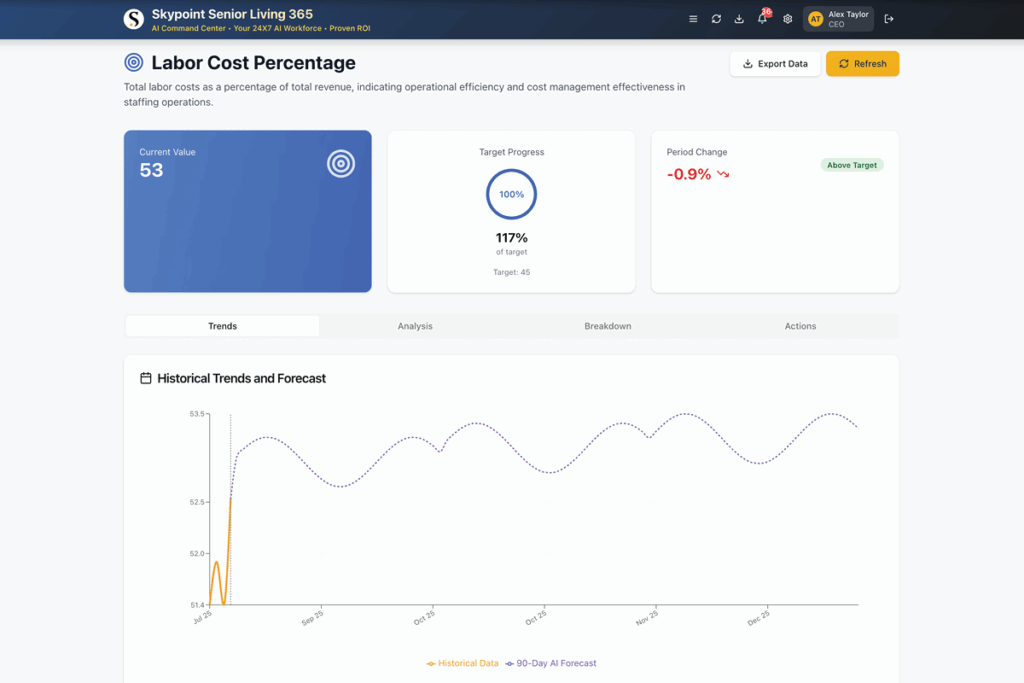
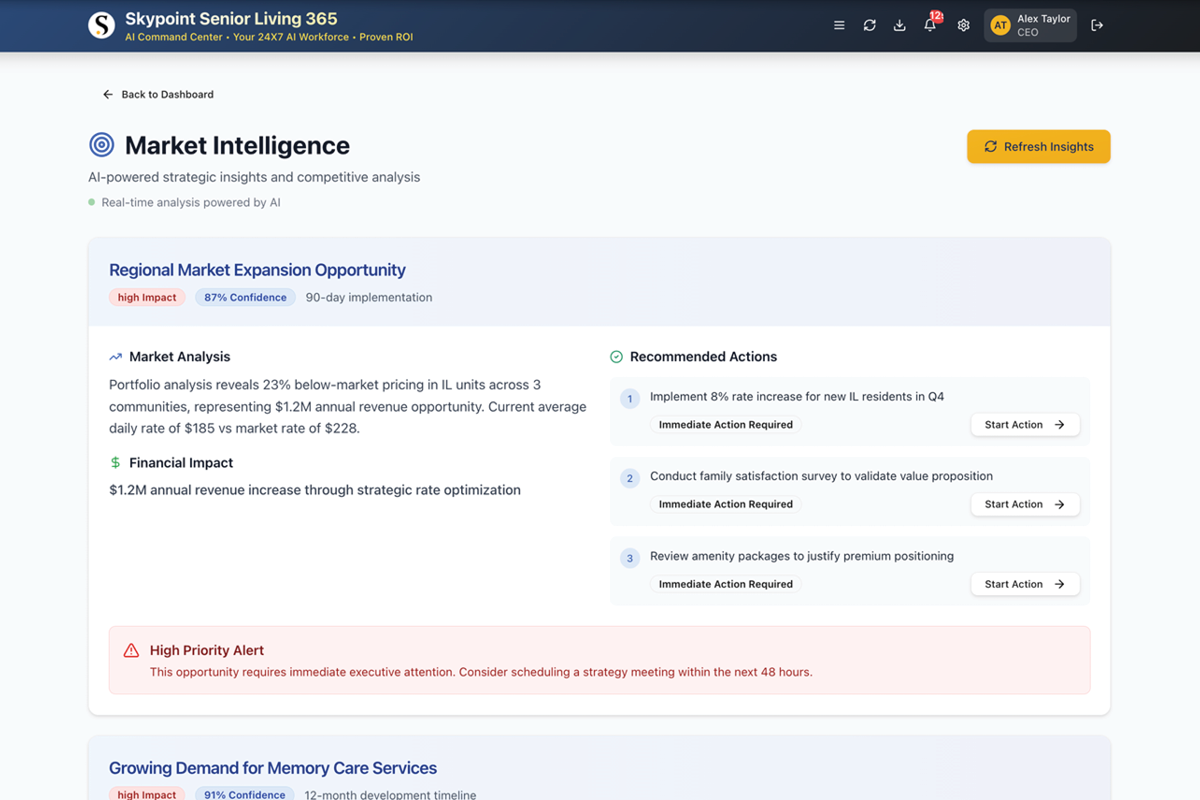
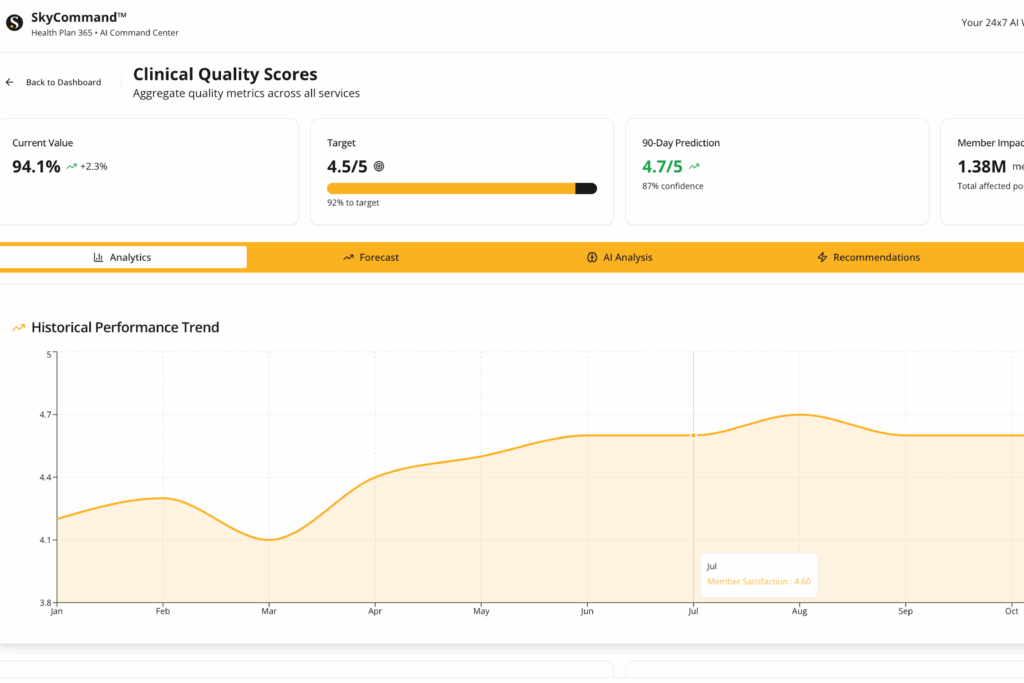
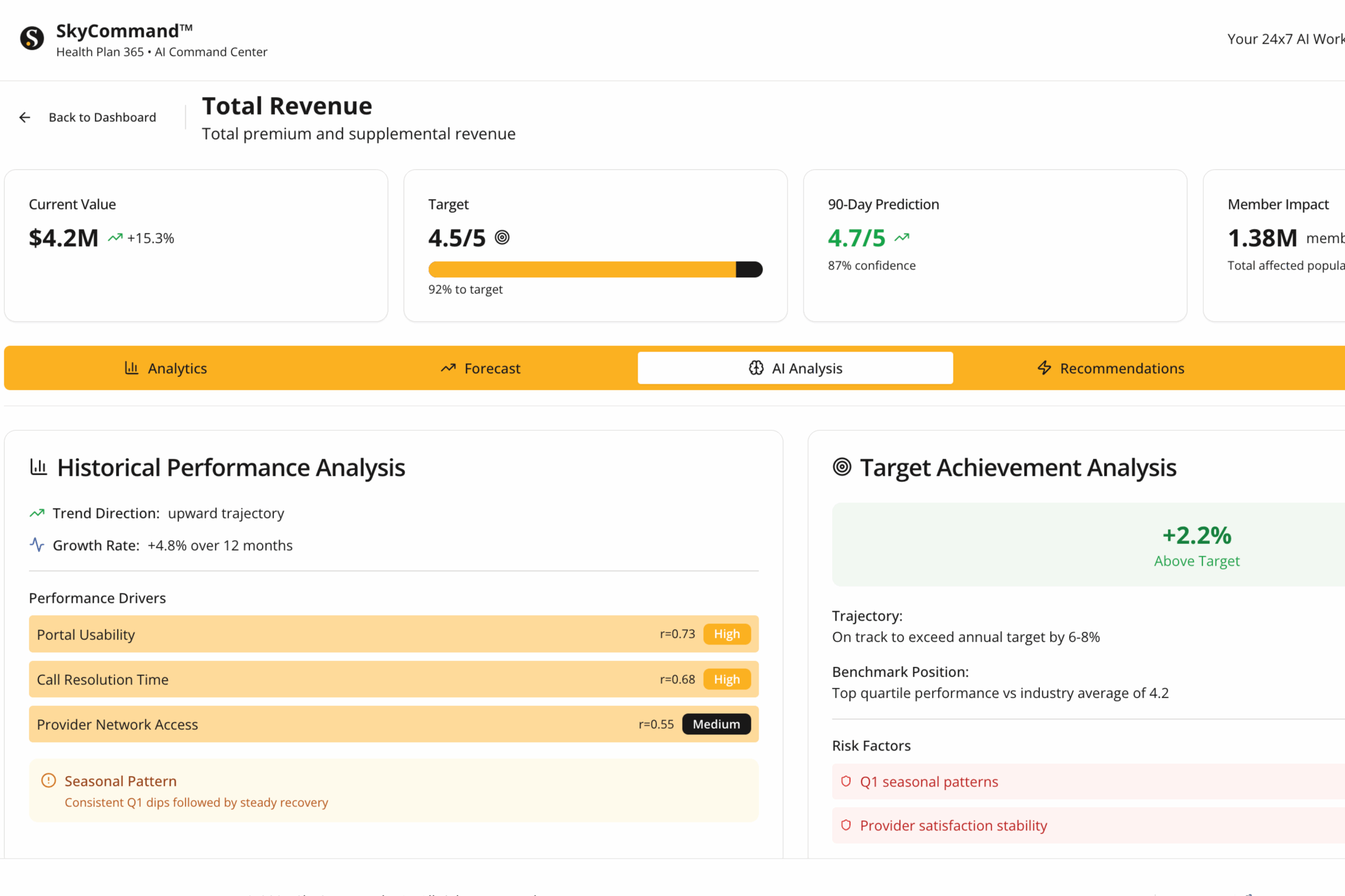
Transform siloed data into actionable intelligence. Skypoint’s AI Platform accelerates data-centric AI initiatives for healthcare, so you see results in weeks, not months.
- Product
The Skypoint AI Platform
Our HITRUST r2 Certified AI Platform for the healthcare industry helps you unify your data, uncover insights, and optimize productivity.
- Resources
Data and AI Resources
Connect with Skypoint at healthcare events, read our customer stories, and catch up on the latest AI developments on our blog.
Training and Events
Resources
- About
Who We Are
Our team of AI and BI experts helps healthcare organizations solve operational inefficiencies and enhance productivity through unified data and industry-specific compound AI systems.
About Skypoint
Contact